We believe that treatments with nanodevices have the potential to dramatically improve treatment of some of the most common neurological and psychiatric illnesses by addressing the underlying causes.
Brian Litt, M.D.

Epilepsy and many other common brain disorders are caused by localized problems in brain networks. And yet, most treatments today work at a macro level.
For example, a disease caused by a select group of neuronal cells in one area of the brain may routinely be treated with medication that floods every tissue in the body and can cause any number of side effects, some serious.
Some implantable treatment technologies have been developed, but they also have side effects and do little to slow the progress of the disease. This is because they are relatively non-specific and fail to focus on what scientists call disease mechanisms.
Getting to the root of the problem.
Neuroscientists now see a possibility for treating epilepsy and other neurological disorders where (and only where) the problems occur, without disturbing other areas in the body. Because treatments would be precisely targeted, to a specific location in the brain and inside certain cells, there is good reason to believe they would be far more effective.
Using nanodevices to repair damaged cells.
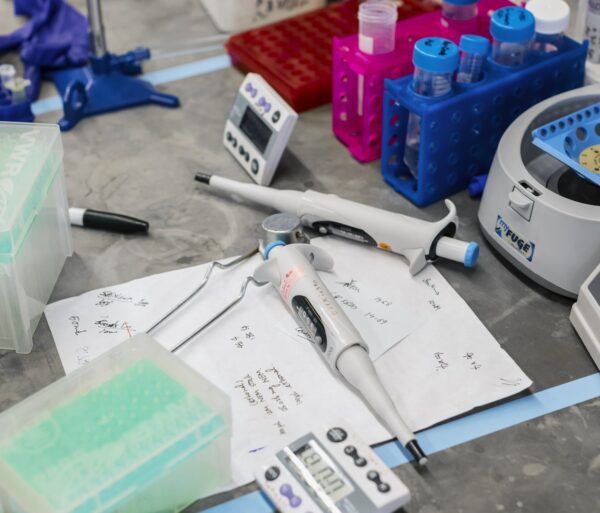
With support from a 2013 BRF Scientific Innovations Award, Brian Litt, M.D., pursued the treatment of epilepsy at the molecular level. Dr. Litt planned to use nanotechnology to develop devices that are smaller than you can see under a conventional microscope, and are programmed to travel to damaged cells and deliver therapeutic agents to repair them.
Mind-boggling possibilities.
Such a device could be coated with biologic particles to keep the immune system from attacking it, and with antibodies or surface protein receptors to guide the device to its destination. Once the target is reached, the device could be “pinged” to release the therapeutic agents it has carried to the damaged cells.
After making the repair, depending on how the device is fabricated it might dissolve; or be engulfed and consumed by micro-organisms preloaded on the device and preprogrammed to clean up; or be excreted.
Implications for multiple diseases.
Dr. Litt’s team has concentrated on the potential for nanodevices designed to treat epilepsy. He believes much of what his research team learns will be applicable to treatments for depression, movement disorders like Parkinson’s and Huntington’s disease, schizophrenia, and possibly even some types of brain tumors.
The promise of neuroscience continues to amaze.