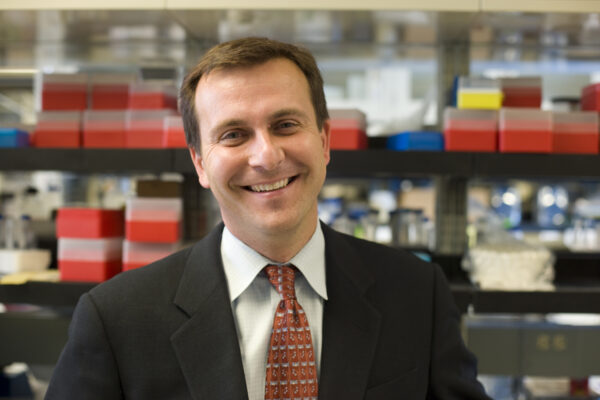
Dr. Maciej Lesniak, Associate Professor of Surgery at The University of Chicago, is working on a novel treatment strategy that will specifically target tumor cells and spare normal cells by manipulating the immune system—immunotherapy. Immunotherapy means a treatment based upon the concept of modulating the immune system to fight disease, in this case destroy tumors.
Brain tumors have been previously considered to exist in an area that restricted immune response. However, recent studies have indicated that the immune system is finely regulated within the brain and that immunotherapeutic approaches could be utilized in the treatment of malignant brain tumors. Dr. Lesniak used his Brain Research Foundation Seed Grant to determine if regulatory T cells (Treg), a component of the immune system, found in malignant gliomas selectively inhibit the host immune response within the CNS and contribute to the rapid progression of brain cancer.
The immune system is a complex group of defense responses that protect against infection by identifying and killing pathogens and tumor cells. An important component of the immune response is specialized white blood cells called T cells. There are a variety of subsets of T cells. Dr. Lesniak’s project studied T cells that expressed the cell-surface glycoproteins CD4 and CD25 and the transcription factor FoxP3. CD4+CD25+FoxP3+ regulatory T cells (Treg) suppress immune responses of other cells. Treg are involved in shutting down immune responses after they have successfully tackled invading organisms and also in keeping in check immune responses that may potentially attack one’s own tissues.
Dr. Lesniak utilized a mouse glioma model to examine the presence of Treg in CNS tumors. He manipulated the immune response by depleting the CD4+CD25+FoxP3+ regulatory T cells (Treg) to determine what effect the absence of Treg would have on intracranial tumor growth and progression. His results showed that Treg are present and in fact elevated in intracranial versus peripheral tumors. It seems this high number of Treg permits the aggressive growth rate seen in malignant brain tumors. When the suppressing effect of Treg is interfered with using an anti-CD25 monoclonal antibody, the immune system is activated and can destroy tumor cells, increasing the survival rate of mice with intracranial tumors.

In addition, Dr. Lesniak demonstrated that Treg progressively infiltrate gliomas with increasing tumor grade (tumor aggressiveness). Heme oxygenase-1 (HO-1), an enzyme that catalyzes the degradation of heme and is induced in response to stress such as oxidative stress, hypoxia and cytokines, has been shown to accumulate during glioma progression and to play a critical role in FoxP3 mediated immune suppression. The expression of FoxP3 and HO-1 was analyzed in patients with different grades of gliomas. It was observed that (1) the highest level of FoxP3 was expressed in patients with the most aggressive gliomas, grade IV; and (2) the expression of HO-1 directly correlates with the expression of FoxP3.
Based on these studies, it is clear that Treg play a role in the rapid progression of brain cancer, and may be an optimal target for new therapies. By interfering with Treg to remove the suppression of the immune system, the immune system will now be able to destroy cancer cells. The ultimate goal would be to design appropriate immunotherapeutic interventions that could be used in clinical applications to increase the survival rate of patients with gliomas.