Goal: to identify a new pain receptor and provide relief to millions of patients that are currently inadequately treated
A person steps on a tack. In a fraction of a second, the peripheral nervous system relays an electrical message telling the brain there is cell and tissue damage. The person feels pain and reacts.
How that electrical messaging works on the cellular level— specifically, how pain-sensing neurons (nociceptors) signal the detection of tissue injury—is the focus of research by Dr. Sean Cook, an assistant professor in the University of Chicago’s Department of Anesthesia and Critical Care.
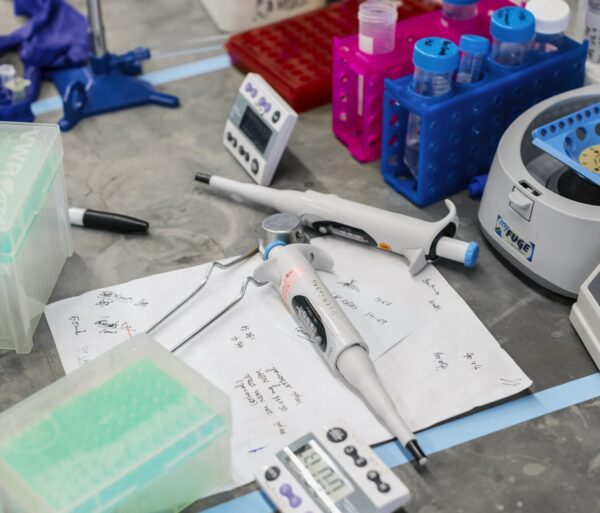
Dr. Cook’s grant from the Brain Research Foundation has allowed him to study a specific ATP (adenosine triphosphate) receptor, identified as P2Y2. Evidence indicates that ATP, found in every cell, is released with cell damage. The P2Y2 receptor, which lies on the surface of nociceptors, reacts immediately to the ATP release, triggering an electrical message that the nervous system interprets as pain. Dr. Cook’s goal is to learn how the P2Y2 receptor works—to uncover its molecular mechanisms that cause the nociceptors to fire.
“Our goal is to prove to the community that this receptor is an important mediator of pain,” Dr. Cook said of P2Y2. “We want to look at what starts and stops the signal, because our hypothesis is that if you can stop the firing of the receptor, you can stop the pain.”
Many current therapies for pain management cause harmful side effects or are not as effective as desired. For example, opiates, including morphine, are extremely effective, but often addictive and with dangerous side effects, including respiratory depression.
Dr. Cook’s research could provide molecular knowledge that someday leads to new and better pain management strategies. He envisions a day when the millions of people who suffer from long-term, chronic pain—such as that from arthritis, diabetes and cancer—would be helped by drugs that prevent nociceptors from firing, thereby blocking pain at its source.
Dr. Cook cautioned that new pain therapies based on blocking receptors are a long way off. His seed grant experiment represents the first basic, academic science look at the P2Y2 receptor’s role in pain.